Global health innovations can be game-changers at home, too

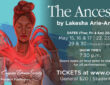
In this picture taken on February 7, 2013 hospital staff shift a patient the Narayana Hrudayalaya cardiac-care hospital in Bangalore. What if hospitals were run like a mix of Wal-Mart and a low-cost airline? The result might be something like the chain of “no-frills” Narayana Hrudayalaya clinics in southern India. Using pre-fabricated buildings, stripping out air-conditioning and even training visitors to help with post-operative care, the group believes it can cut the cost of heart surgery to an astonishing 800 USD. AFP PHOTO/Manjunath KIRAN (Photo credit should read Manjunath Kiran/AFP/Getty Images)
By , , , , , , and
Rich and poor countries used to struggle with different sets of health issues: obesity in one versus malnutrition in the other; heart disease and cancer as leading causes of death in rich countries, deaths from infection topping the list in poor countries.
That is changing. India and China each have more people with diabetes and obesity than does the United States, while Zika and other tropical diseases have come ashore here. Lengthening life spans around the world ensures that cancer and dementia impose huge burdens on health care systems at home and abroad. Equally important, both rich and poor countries face the challenge of making health care affordable: High costs impede access to health care in poor countries, and rich countries worry that their skyrocketing health care costs are unsustainable — in the United States, health spending is projected to grow at an average annual rate of 5.8 percent until 2025.
This global convergence of health issues calls for universal solutions. It has begun reshaping how we think about health care innovation. For decades, health care expertise and investment flowed in one direction, from rich countries to poor countries. That is no longer the case. Take, for example, an effort by Ascension Health — America’s largest nonprofit health system — to change its approach to patient care. For more than a year, Ascension has been sending patients who need open heart surgery and hip replacement to a hospital in the Cayman Islands run by Narayana Health. This Bangalore-based health care group is best known for providing inexpensive heart surgery to India’s poor. Its doctors perform these procedures at a fraction of what they costin the US.
There is more to this partnership than outsourcing. Ascension is rotating doctors and other professionals from its mainland hospitals through the Cayman Islands facility, where they observe Narayana Health’s model of delivering high-quality, affordable services. One Ascension executive saw the facility as an offshore “convening point” for health care innovation in the United States.
This partnership, which illustrates how a developed country’s health care system can look to a developing country for solutions, should be more widely celebrated. Unfortunately, innovations that emerge in developing countries tend to be labeled as solutions for “global health.” But that term has a specific — and possibly misleading — connotation in the United States. When the Kaiser Family Foundation surveyed the American public on its attitudes toward global health, it asked about America’s role in improving health for people in developing countries, not about applying lessons from developing countries to problems at home, or about finding solutions to common challenges.
The research community is looking past this distinction between local and global health. Scientists in the United States, for example, are using gene-editing tools like CRISPR-Cas9 to create rapid, portable, low-cost diagnostics for the Zika virus. This work is intended to have an impact on lives halfway around the world, but will also improve the lives of those close to home. Faster ways to diagnose Zika could well serve pregnant women in the American South, who anxiously wait for weeks to get test results that tell them if their unborn babies are at risk of serious Zika-related birth defects.
Technologies coming out of projects traditionally branded as global health could be game-changers for outcomes in the United States as well. But will these technologies ever realize their capacity? Will they remain viable through the processes of scale-up and commercialization, particularly in high-resource countries?
Questions like those are increasingly being asked of any project seeking funding, as public, private and philanthropic investors are shifting away from traditional philanthropy and toward outcome-driven global health ventures. Billionaires like Bill Gates and Mark Zuckerberg are committing huge portions of their wealth toward result-driven global health research. Leading world economists are proclaiming the impressive economic returns projected for global health innovations as they call for more investment in this sector. Investment funds are being set up specifically for impact capital, and they guide those who want to invest in projects that not only have an impact in developing countries but provide financial returns as well. Educational centers like the Massachusetts Institute of Technology’s D-Lab and Media Lab and Stanford University’s SCID and d.school are responding by training designers and engineers to build global health tools complete with a sustainable business and scale-up plan.
The collaboration between Ascension and Narayana Health, the work on improving Zika diagnostics, and the shift toward result-driven global health research all have something in common: They recognize that in a world where health issues in rich and poor countries are becoming more similar, innovation should know no borders. Health care solutions that emerge in developing countries, or that are researched and funded in the United States but aimed at developing countries, could help address health care challenges here in the United States.
As active participants in Boston’s life sciences ecosystem, we believe that the faster we can do away with the distinction between “global health” and our “local” health care system — in the public perception, as well as among researchers, policymakers, businesses, and philanthropists — the better our chances of finding sustainable solutions to health care challenges everywhere in the world.
Aikaterini Mantzavinou, Bryan J. Ranger, Emma Costa, Samuel Rodriques, and Hok Hei Tam are students at MIT and cofounders of the MIT Cost-effective Health care Initiative. Rajarshi Banerjee is an associate at Ropes & Gray LLP. Lindsay Brownell is an MIT alumna and freelance science writer.
For more on this story go to: https://www.statnews.com/2017/03/14/health-care-global-united-states/